High-intensity focused ultrasound (HIFU)
What is HIFU?
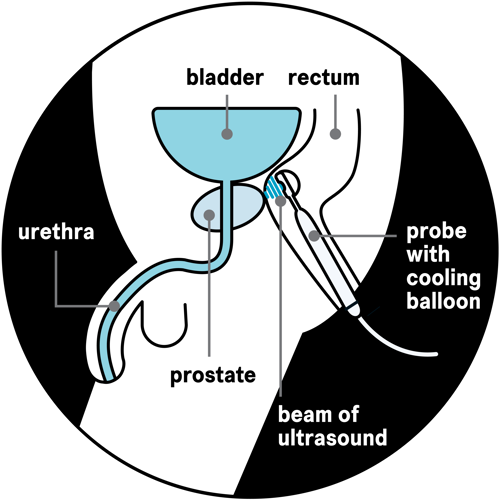
High-intensity focused ultrasound (HIFU) uses high-frequency ultrasound energy to heat and destroy cancer cells in the prostate. A beam of ultrasound energy travels into the prostate from a probe put into the back passage (rectum).
There are two types of HIFU:
- focal HIFU, which treats areas of cancer in the prostate and a small area around them
- whole-prostate HIFU, which treats the whole prostate.
Ask your doctor or nurse which treatment might be suitable for you.
In the UK, HIFU is available either in specialist centres or as part of a clinical trial. This is because it is newer than some other treatments, so we still need to know more about the side effects and how well it works in the long term.
If HIFU isn't available at your local hospital, you can ask your doctor to refer you to another hospital in the UK that does offer it.
Watch our video on high-intensity focused ultrasound to find out more:
Who can have HIFU?
The stage and grade of your prostate cancer helps your doctor decide if HIFU is a suitable treatment option for you.
HIFU might be suitable for you if your cancer hasn’t spread outside your prostate (localised prostate cancer).
HIFU is sometimes an option if your prostate cancer has started to break out of your prostate, has spread to the area just outside the prostate (locally advanced prostate cancer) or has a higher risk of spreading. But your cancer may be more likely to come back after treatment than in men with localised cancer.
HIFU isn't an option if your cancer has spread outside your prostate to other parts of your body (advanced or metastatic prostate cancer).
HIFU can also be used to treat cancer that has come back after previous radiotherapy (recurrent prostate cancer). This is called salvage HIFU.
If your cancer comes back after your first HIFU treatment, you may be offered another session. You may hear this called repeat or redo HIFU.
HIFU can also be an option if you have had cryotherapy or irreversible electroporation (Nanoknife™) before as your first treatment.
HIFU may not be suitable if you have a large prostate. Focal HIFU may still be an option if the areas of cancer are close enough to the probe for the ultrasound to treat. Your scan and biopsy results will show whether this is the case.
In some cases, you might need to have another treatment first to shrink the prostate or to reduce the risk of some urinary problems after HIFU. These include:
Speak to your doctor about whether HIFU is a suitable option for you and whether it’s available in your area.
Read more about other treatment options for prostate cancer.
What are the advantages and disadvantages of HIFU?
Everyone's experience of prostate cancer is different and what may be important for one person may be less important for someone else. If you're offered HIFU, speak to your doctor or nurse before deciding whether to have it. They can help you decide if it's right for you.
Take time to think about whether you want to have HIFU. We've included a list of questions that you might find helpful. You can also ask about any other treatments that might be available.
Advantages
- HIFU doesn’t involve any cuts to the skin or needles, apart from a needle in your hand to give you a general anaesthetic.
- Focal HIFU can treat small areas of cancer while causing little damage to nearby tissue, nerves and muscles.
- You only need a short hospital stay – you can usually go home on the same day as your treatment.
- Recovery is usually quick and most men get back to their normal, gentle daily activities within two weeks.
- HIFU is less likely than surgery to cause erection or urinary problems.
- You may be able to have HIFU if your cancer has come back after radiotherapy.
- You may be able to have HIFU again if your cancer comes back after your first HIFU treatment. This isn’t the case with all treatments.
- You may also be able to have other treatments after HIFU if your cancer comes back, such as surgery or radiotherapy.
Disadvantages
- You might get side effects such as erection and urinary problems. But focal HIFU may cause fewer side effects than surgery, radiotherapy and whole-prostate HIFU.
- Compared with other treatments, we don’t know how well it works in the longer term (after 10 years).
- HIFU may not be suitable if you have a large prostate. But it may still be an option if you have another treatment to shrink your prostate first.
- HIFU isn’t widely available in the UK and you may need to travel a long way to your nearest treatment centre.
What does HIFU involve?
Each hospital will do things slightly differently. We’ve included some general information about what might happen before, during and after HIFU. Your doctor or nurse will give you more information about your treatment.
Before your treatment
If you’re thinking of having focal HIFU, you will usually go to a screening appointment first. You’ll have a magnetic resonance imaging (MRI) scan, which produces detailed images of the prostate and shows the location of the cancer.
You may also have a prostate biopsy, if your doctor needs more information about where the cancer is and how likely it is to grow and spread outside the prostate. These tests will confirm whether HIFU is suitable for you and will help your surgeon target the area of the prostate that needs to be treated.
During your treatment
On the morning of your HIFU treatment, you’ll be given an enema to empty your bowels. This makes it easier for the doctor to see clear images of your prostate. An enema is a liquid medicine that is put inside your back passage (rectum). You’ll also be asked not to eat or drink for around six hours before the HIFU treatment.
You will usually have a general anaesthetic so that you’re asleep during the treatment.
During your treatment, you will need to lie on your back with your legs apart. You may have a catheter put in to drain urine (wee) out of your bladder. A catheter is a thin tube that is passed into your bladder, either up your penis or through the wall of your lower abdomen (stomach area).
Your surgeon will place a probe inside your back passage (rectum). The probe gives out a beam of high-intensity ultrasound energy, which travels through the wall of the back passage into the prostate. The beam treats one small area of the prostate at a time – the size of a grain of rice.
Your surgeon will plan your treatment so the HIFU machine moves the beam around, heating and destroying the cancer cells in the area being treated.
The probe also uses ultrasound to create images of the prostate after each area is treated. This helps the surgeon target the cancer and avoid healthy tissue like the urethra, which is the tube you urinate (wee) through.
The probe is surrounded by a cooling balloon so that the heat doesn’t damage your back passage.
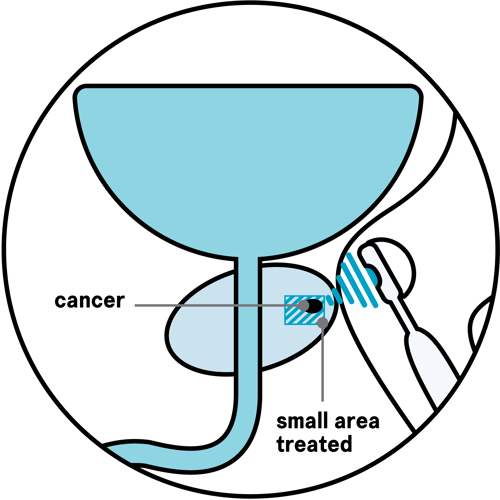
You may also hear focal HIFU called focal therapy or partial ablation with HIFU. It is the most common type of HIFU used in the UK. It treats only the areas of cancer in the prostate and takes one to two hours. It may be suitable for men who only need to have some of their prostate treated.
Your surgeon will treat the areas of cancer that need treating and a small area around them called a margin. Less of the healthy tissue is damaged during focal HIFU compared to whole-prostate HIFU.
Some men who have focal HIFU have only one area of cancer in their prostate.
Other men have more than one area of cancer in their prostate, but some areas that have low-risk cancer are not treated on purpose (see diagram below). This is because low-risk cancer is less likely to spread and it may never cause any problems or affect how long you live. These men will have regular tests to keep an eye on the cancer that is not treated.
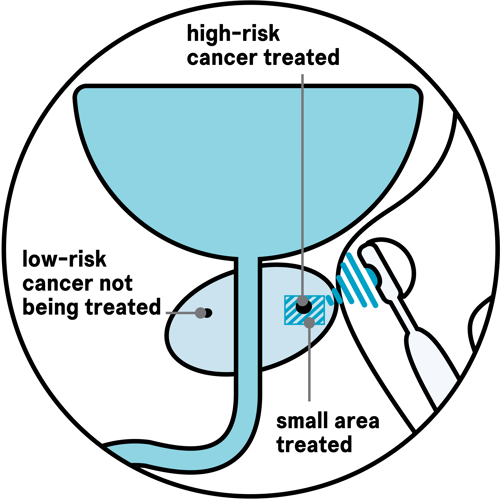
With focal HIFU, there is a small risk that some areas of cancer that do need treating may be missed if they weren’t picked up by the scan and biopsy. If this happens, there are further treatments that you can have.
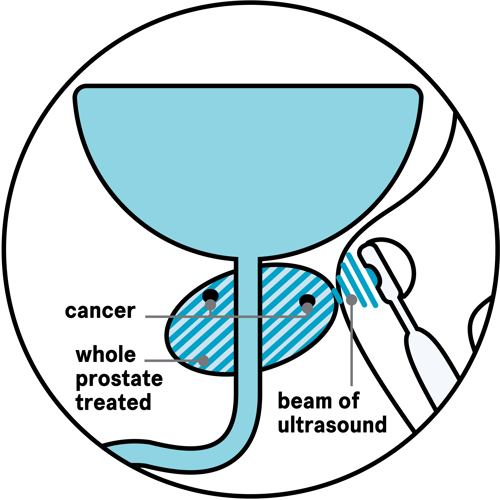
Whole-prostate HIFU treats the whole of the prostate and takes two to three hours.
It is less common than focal HIFU, but may be suitable for men who have cancer that needs treating in more than one or two areas of their prostate. It may also be an option for those who can't or choose not to have other treatments such as surgery or radiotherapy.
After your treatment
You should be able to go home on the same day as your treatment. Your doctor or nurse will check that you’ve recovered from the anaesthetic and are fit to go home. You shouldn’t drive for 24 to 48 hours after the anaesthetic. Ask a family member or friend to take you home.
You may have pain in the area between your testicles and back passage, but you’ll be given pain-relieving medicine to take at home if you need them.
You will also get antibiotics to prevent infection and may be given a medicine called a laxative to help you empty your bowels.
HIFU usually causes the prostate to swell to begin with, which can make it difficult to urinate. You’ll have a catheter to drain urine from your bladder until the swelling has gone, usually for up to a week after treatment.
Before you go home your doctor or nurse will show you how to look after your catheter. They’ll also give you an appointment to have your catheter removed.
What happens afterwards?
You will have check-ups with your doctor or nurse at the hospital at first, and then with your GP. This is often called follow-up. The aim is to:
- check how your cancer has responded to treatment
- deal with any side effects of treatment
- give you a chance to raise any concerns or ask any questions.
You will have a PSA blood test every three to six months for the first few years to check how well the HIFU has worked. The PSA test is a blood test that measures the amount of a protein called PSA in your blood. Your PSA is likely to reach its lowest level a few months after HIFU.
You may also have an MRI scan to check that your treatment has worked as intended.
If you have focal HIFU, you might have low-risk cancer in another area of the prostate that is not treated on purpose. You will have regular tests to monitor the cancer that isn't treated. These may include PSA blood tests, MRI scans, and prostate biopsies.
Your PSA levels may go up straight after treatment with HIFU. This is because the treatment will cause inflammation in your prostate, which can cause an increase in PSA levels. But your PSA levels should go down and stay low after about six months, once your prostate has healed. After a year, a continuous rise in your PSA level could be a sign that your cancer has come back. If this happens, your doctor may suggest you have further tests, such as an MRI scan and a biopsy.
Sometimes they might also suggest other types of scans, to see if the cancer has spread to other parts of your body. If you need other scans, your doctor or nurse will tell you more about these.
If your cancer does come back, your doctor will talk to you about further treatment options. You may be offered:
- more HIFU
- external beam radiotherapy
- permanent seed brachytherapy or high dose- rate brachytherapy
- cryotherapy
- irreversible electroporation
- surgery (radical prostatectomy)
- hormone therapy.
Or your doctor may suggest monitoring your cancer, rather than treating it straight away.
Read more about what happens if your cancer comes back and what treatments might be available.
What are the side effects of HIFU?
Like all treatments, HIFU can cause side effects. These will affect each person differently, and you might not get all of them.
The most common side effects are urinary problems and difficulty getting or keeping an erection (erectile dysfunction).
Having HIFU more than once may increase your risk of urinary problems or erectile dysfunction, but it shouldn't increase your risk of other side effects.
Less of the healthy tissue is damaged during focal HIFU than with whole-prostate HIFU, so there’s a lower risk of side effects such as urinary and erection problems.
If you have hormone therapy, a TURP or laser treatment as well as HIFU, these can also cause side effects.
Read more about these side effects in our information on hormone therapy, and enlarged prostate.
Ask your doctor or nurse for more information about your risk of side effects. They may be able to show you results of treatments they’ve carried out and put you in touch with other men who’ve had HIFU.
Short-term side effects
These can develop soon after your treatment and may include:
You might see some blood in your urine while the catheter is in place. You might also see some small pieces of prostate tissue in your urine for six to eight weeks after HIFU. This is normal. If you are worried or see signs of an infection, lots of blood clots in your urine, or bright red blood every time you urinate, then go to A&E straight away.
Some men have problems getting or keeping an erection (erectile dysfunction) after HIFU. This is because it can damage the blood vessels and nerves that control erections. For some men this will improve, but for others this will be a longer-term side effect of HIFU. There are treatments that can help with erection problems.
Some men get a urine infection after HIFU. Signs of a possible urine infection include:
- a fever (high temperature)
- feeling shivery
- a burning feeling when you urinate
- dark or cloudy urine with a strong smell
- needing to urinate more often than usual.
Tell your doctor or nurse if you have any signs of a urine infection. They’ll usually give you antibiotics to treat the infection.
Some men need to urinate more often than usual after HIFU. This is called urinary frequency and usually gets better over time.
Some men find it hard to empty their bladder properly after their catheter is removed – this is called urine retention. You may be given a type of drug called an alpha-blocker to help you pass urine (wee). These are tablets that help to relax the muscles in the prostate and around the opening of the bladder, making it easier to urinate.
After HIFU, the treated prostate tissue can block the urethra. If your flow of urine is weak or slow after your catheter is taken out, speak to your doctor or nurse.
If you can’t urinate at all, call your doctor or nurse straight away or go to your nearest accident and emergency (A&E) department. They may need to drain your bladder using a catheter.
They might also suggest using a temporary catheter (self-catheterisation). This is where you put a catheter in yourself when you want to urinate and take it out afterwards. Some men find that urinary problems improve over a few weeks, but other men need further treatment to clear the blockage.
Some men get an infection in the testicles or the tubes that carry sperm from the testicles. Signs of a possible infection include pain, swelling, warmth and tenderness in one or both testicles. Tell your doctor or nurse if you have any of these symptoms. They’ll usually give you antibiotics to treat the infection.
Some men feel extreme tiredness (fatigue) after having HIFU. Fatigue can affect your everyday life. It can affect your energy levels, your motivation and your emotions – which can be hard to cope with. As HIFU is quite a new treatment, we don’t yet know how long fatigue may last for.
We have lots of information on our website to help you manage fatigue. Our Specialist Nurses also offer fatigue support. They can talk to you in depth about your experience of fatigue, the impact it is having on day-to-day life and discuss ways to better manage your tiredness.
Longer-term side effects
Most side effects will settle down after HIFU, but some men have longer-term side effects or problems that develop later. The risk of longer-term side effects is lower after focal HIFU than after whole-prostate HIFU. They may include:
Some men find that their erection problems don't improve over time. There are treatments that can help manage erection problems.
You should still be able to orgasm (climax), but you might release less semen (the fluid that carries sperm), or no semen at all. This means you may not be able to have children naturally after treatment. If you’re planning to have children, you might be able to store your sperm before HIFU to use in fertility treatment. If this is important to you, ask your doctor or nurse about it.
Talk to your doctor or nurse if you have problems with erections or other sexual problems. They can explain your treatment options and arrange free treatment on the NHS. They can also refer you to an erectile dysfunction (ED) clinic.
Our Specialist Nurses also offer a telephone service supporting people with sexual problems after treatment for prostate cancer. They can talk to you about the impact of treatment on your sex life and relationships, and discuss possible treatments or ways to deal with these changes.
Read more about sexual problems and how to manage them.
HIFU can cause longer-term urinary problems. You may have some of the following problems straight after treatment, or they might develop some time later.
- You may leak urine (urinary incontinence) after HIFU. This is more likely if you’ve already had external beam radiotherapy.
- If your urethra, which is the tube you urinate through, or the opening of your bladder becomes narrow (a stricture), you may find it difficult to empty your bladder.
Talk to your doctor or nurse if you have any urinary problems. There are things that can help, including lifestyle changes, pelvic floor muscle exercises and treatments. Your doctor or nurse may also refer you to an NHS continence service, run by nurses and physiotherapists who specialise in urinary problems.
Very rarely, HIFU can cause a hole between the back passage (rectum) and the urethra. This is called a rectal fistula. It affects fewer than 1 in 500 men who have focal or whole-prostate HIFU (less than one per cent). It may be slightly more likely if you’ve already had radiotherapy.
Signs of a possible rectal fistula include:
- urine coming out of your back passage
- pain in your pelvis or back passage
- bowel contents in your urine
- air bubbles in your urine
- urine infections, but these can also be caused by other things.
Talk to your doctor or nurse straightaway if you think you may have a rectal fistula. They may suggest waiting to see if the fistula heals by itself. You may have a catheter (a thin tube that drains urine out of your body) for about three to six months to give the fistula time to heal. Or you may need an operation to repair the hole.
Dealing with prostate cancer
Being diagnosed with prostate cancer can change the way you think and feel about life. It’s normal to feel scared, worried, stressed, helpless or even angry. Lots of men with prostate cancer get these kinds of thoughts and feelings. But there’s no ‘right’ way to feel and everyone reacts in their own way. Our wellbeing hub has information to help support you in looking after your emotional, mental, and physical wellbeing.
Finding out about things you can do to help yourself can help you to feel more in control. Families can also find this a difficult time and they may need support and information too. If you are close to someone with prostate cancer, find out more about how you can support someone with prostate cancer and where to get more information.
Questions to ask your doctor or nurse
You may find it helpful to keep a note of any questions you have to take to your next appointment.
- What are the advantages and disadvantages of HIFU?
- Where is this treatment available?
- Can I see the results of HIFU treatments you have carried out?
- What are my other treatment options?
- Will I have focal HIFU or whole-prostate HIFU?
- What are the side effects of HIFU? How likely am I to get them?
- How can I manage any side effects I get?
- How will I know if the treatment has worked?
- How likely is it that I’ll need more treatment after HIFU?
- What treatments are available after HIFU?
References and reviewers
Updated: July 2025 | To be reviewed: July 2028
- Abufaraj M, Siyam A, Ali MR, Suarez-Ibarrola R, Yang L, Foerster B, et al. Functional Outcomes after Local Salvage Therapies for Radiation-Recurrent Prostate Cancer Patients: A Systematic Review. Cancers. 2021 Jan 11;13(2):244.
- Bakavicius A, Marra G, Macek P, Robertson C, Abreu AL, George AK, et al. Available evidence on HIFU for focal treatment of prostate cancer: a systematic review. Int braz j urol. 2022 Apr;48(2):263–74.
- Bonkat G RB, Bruyère F, Geerlings SE, Koves B, Schubert S, Pilatz A, et al. EAU Guidelines on Urological Infections [Internet]. European Association of Urology; 2024. Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-Guidelines-on-Urological-Infections-2024.pdf
- Bourke L, Smith D, Steed L, Hooper R, Carter A, Catto J, et al. Exercise for Men with Prostate Cancer: A Systematic Review and Meta-analysis. European Urology. 2016 Apr;69(4):693–703.
- Cornford P, Tilki D, Van Den Bergh RCN, Briers E. EAU Guidelines on Prostate Cancer [Internet]. European Association of Urology; 2024 [cited 2025 Jan 16]. Available from: https://d56bochluxqnz.cloudfront.net/documents/full-guideline/EAU-EANM-ESTRO-ESUR-ISUP-SIOG-Guidelines-on-Prostate-Cancer-2024_2024-04-09-132035_ypmy_2024-04-16-122605_lqpk.pdf
- Crouzet S, Rouviere O, Martin X, Gelet A. High-intensity focused ultrasound as focal therapy of prostate cancer: Current Opinion in Urology. 2014 May;24(3):225–30.
- Dickinson L, Arya M, Afzal N, Cathcart P, Charman SC, Cornaby A, et al. Medium-term Outcomes after Whole-gland High-intensity Focused Ultrasound for the Treatment of Nonmetastatic Prostate Cancer from a Multicentre Registry Cohort. European Urology. 2016 Oct;70(4):668–74.
- Gardner JR, Livingston PM, Fraser SF. Effects of Exercise on Treatment-Related Adverse Effects for Patients With Prostate Cancer Receiving Androgen-Deprivation Therapy: A Systematic Review. Journal of Clinical Oncology. 2014 Feb 1;32(4):335–46.
- Golan R, Bernstein AN, McClure TD, Sedrakyan A, Patel NA, Parekh DJ, et al. Partial Gland Treatment of Prostate Cancer Using High-Intensity Focused Ultrasound in the Primary and Salvage Settings: A Systematic Review. The Journal of Urology. 2017 Nov;198(5):1000–9.
- Guang ZLP, Kristensen G, Røder A, Brasso K. Oncological and Functional Outcomes of Whole-Gland HIFU as the Primary Treatment for Localized Prostate Cancer: A Systematic Review. Clinical Genitourinary Cancer. 2024 Aug;22(4):102101.
- Guillaumier S, Peters M, Arya M, Afzal N, Charman S, Dudderidge T, et al. A Multicentre Study of 5-year Outcomes Following Focal Therapy in Treating Clinically Significant Nonmetastatic Prostate Cancer. European Urology [Internet]. 2018 Jun [cited 2018 Jul 9]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S0302283818304317
- Guy’s and St Thomas’ NHS Foundation Trust. High-intensity focused ultrasound to treat prostate cancer [Internet]. Guy’s and St Thomas’ NHS Foundation Trust. 2022 [cited 2025 Mar 24]. Available from: https://www.guysandstthomas.nhs.uk/health-information/hifu-to-treat-prostate-cancer/recovery
- Hatiboglu G, Popeneciu IV, Deppert M, Nyarangi-Dix J, Hadaschik B, Hohenfellner M, et al. Quality of life and functional outcome after infravesical desobstruction and HIFU treatment for localized prostate cancer. BMC Urol [Internet]. 2017 Jan 11 [cited 2018 Aug 16];17. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5225650/
- Hechtman LM. Clinical Naturopathic Medicine [Internet]. Harcourt Publishers Group (Australia); 2014 [cited 2015 Jul 21]. 1610 p. Available from: http://www.bookdepository.com/Clinical-Naturopathic-Medicine-Leah-Hechtman/9780729541923
- Henson CC, Burden S, Davidson SE, Lal S. Nutritional interventions for reducing gastrointestinal toxicity in adults undergoing radical pelvic radiotherapy. Cochrane Database of Systematic Reviews [Internet]. 2013 [cited 2014 Nov 18];(11). Available from: http://doi.wiley.com/10.1002/14651858.CD009896.pub2
- Keilani M, Hasenoehrl T, Baumann L, Ristl R, Schwarz M, Marhold M, et al. Effects of resistance exercise in prostate cancer patients: a meta-analysis. Supportive Care in Cancer. 2017 Jun 10;
- Keogh JWL, MacLeod RD. Body Composition, Physical Fitness, Functional Performance, Quality of Life, and Fatigue Benefits of Exercise for Prostate Cancer Patients: A Systematic Review. Journal of Pain and Symptom Management. 2012 Jan;43(1):96–110.
- Larkin D, Lopez V, Aromataris E. Managing cancer-related fatigue in men with prostate cancer: A systematic review of non-pharmacological interventions. International Journal of Nursing Practice. 2014 Oct;20(5):549–60.
- Lee HS, Song SH, Lee H, Hong SK. Whole gland versus partial gland ablation in patients with localized prostate cancer treated by high-intensity focused ultrasound ablation. Prostate International. 2024 Dec;12(4):213–8.
- Lovegrove C, Peters M, Guillaumier S, Arya M, Afzal N, Dudderidge T, et al. Evaluation of functional outcomes after a second focal high-intensity focused ultrasonography (HIFU) procedure in men with primary localized, non-metastatic prostate cancer: results from the HIFU Evaluation and Assessment of Treatment (HEAT) registry. BJU International. 2020;125:853–60.
- Marra G, Marquis A, Suberville M, Woo H, Govorov A, Hernandez-Porras A, et al. Surveillance after Focal Therapy – a Comprehensive Review. Prostate Cancer Prostatic Dis [Internet]. 2024 Oct 4 [cited 2025 Jan 22]; Available from: https://www.nature.com/articles/s41391-024-00905-0
- Marshall S, Taneja S. Focal therapy for prostate cancer: The current status. Prostate International. 2015 Jun;3(2):35–41.
- Menichetti J, Villa S, Magnani T, Avuzzi B, Bosetti D, Marenghi C, et al. Lifestyle interventions to improve the quality of life of men with prostate cancer: A systematic review of randomized controlled trials. Critical Reviews in Oncology/Hematology. 2016 Dec;108:13–22.
- National Institute for Clinical Excellence. High-intensity focused ultrasound for prostate cancer. Interventional procedure guidance 118. 2005.
- National Institute for Health and Care Excellence. Irreversible electroporation for treating prostate cancer [Internet]. 2023. Available from: https://www.nice.org.uk/guidance/ipg768
- National Institute for Health and Care Excellence. Prostate cancer: diagnosis and management [Internet]. 2021 [cited 2025 Jan 19]. Available from: https://www.nice.org.uk/guidance/ng131
- National Institute for Health and Clinical Excellence. Focal therapy using high-intensity focused ultrasound for localised prostate cancer (Interventional procedures guidance) [Internet]. 2023. Available from: https://www.nice.org.uk/guidance/ipg756/resources/focal-therapy-using-highintensity-focused-ultrasound-for-localised-prostate-cancer-pdf-1899876344182981
- National Institute for Health and Clinical Excellence. Focal therapy using high-intensity focused ultrasound for localised prostate cancer. NICE interventional procedure guidance 424. 2012.
- Epididymitis [Internet]. nhs.uk. 2024 [cited 2025 Feb 11]. Available from: https://www.nhs.uk/conditions/epididymitis/
- Nicoletti R, Alberti A, Castellani D, Yee CH, Zhang K, Poon DMC, et al. Functional outcomes and safety of focal therapy for prostate cancer: a systematic review on results and patient-reported outcome measures (PROMs). Prostate Cancer Prostatic Dis. 2024 Dec;27(4):614–22.
- Pan Y, Wang S, Liu L, Liu X. Whole-gland high-intensity focused ultrasound ablation and transurethral resection of the prostate in the patients with prostate cancer: A systematic review and meta-analysis. Front Oncol. 2022 Oct 12;12:988490.
- Pettersson A, Johansson B, Persson C, Berglund A, Turesson I. Effects of a dietary intervention on acute gastrointestinal side effects and other aspects of health-related quality of life: A randomized controlled trial in prostate cancer patients undergoing radiotherapy. Radiotherapy and Oncology. 2012 Jun;103(3):333–40.
- Poitevin M, Ferragu M, Bigot P, Culty T, Venara A. Rectourethral fistulas after treatment for prostate carcinoma: Update and new management algorithm. Journal of Visceral Surgery. 2025 Feb;S1878788625000104.
- Rahman SN, Kim HS, Webb LT, Diaz GM, Leapman MS, Sprenkle PC, et al. Management strategies for radio-recurrent prostate cancer: a comprehensive review. Transl Cancer Res. 2024 Nov;13(11):6473–88.
- Rakauskas A, Marra G, Heidegger I, Kasivisvanathan V, Kretschmer A, Zattoni F, et al. Focal Therapy for Prostate Cancer: Complications and Their Treatment. Front Surg. 2021 Jul 12;8:696242.
- Ramsay CR, Adewuyi TE, Gray J, Hislop J, Shirley MD, Jayakody S, et al. Ablative therapy for people with localised prostate cancer: a systematic review and economic evaluation. Health Technology Assessment. 2015 Jul;19(49):1–490.
- Reddy D, Peters M, Shah TT, Van Son M, Tanaka MB, Huber PM, et al. Cancer Control Outcomes Following Focal Therapy Using High-intensity Focused Ultrasound in 1379 Men with Nonmetastatic Prostate Cancer: A Multi-institute 15-year Experience. European Urology. 2022 Apr;81(4):407–13.
- Shoji S, Koizumi N, Yuzuriha S, Kano T, Ogawa T, Nakano M, et al. Development and future prospective of treatment for localized prostate cancer with high-intensity focused ultrasound. J Med Ultrasonics [Internet]. 2022 Jan 15 [cited 2025 Jan 21]; Available from: https://link.springer.com/10.1007/s10396-021-01183-2
- Teleni L, Chan RJ, Chan A, Isenring EA, Vela I, Inder WJ, et al. Exercise improves quality of life in androgen deprivation therapy-treated prostate cancer: systematic review of randomised controlled trials. Endocr Relat Cancer. 2016 Jan 2;23(2):101–12.
- Tillisch K. Complementary and alternative medicine for functional gastrointestinal disorders. Gut. 2006 May 1;55(5):593–6.
- Wedlake LJ, Shaw C, Whelan K, Andreyev HJN. Systematic review: the efficacy of nutritional interventions to counteract acute gastrointestinal toxicity during therapeutic pelvic radiotherapy. Alimentary Pharmacology & Therapeutics. 2013 Jun;37(11):1046–56.
- Wolin KY, Luly J, Sutcliffe S, Andriole GL, Kibel AS. Risk of Urinary Incontinence Following Prostatectomy: The Role of Physical Activity and Obesity. The Journal of Urology. 2010 Feb;183(2):629–33.
- Yang CH, Barbulescu DV, Marian L, Tung MC, Ou YC, Wu CH. High-Intensity Focus Ultrasound Ablation in Prostate Cancer: A Systematic Review. JPM. 2024 Dec 20;14(12):1163.
- Hashim Ahmed, Professor of Urology & Consultant Urological Surgeon, Imperial College Healthcare NHS Trust
- Tim Dudderidge, Consultant Urological Surgeon, Spire Southampton Hospital
- Taimur Shah, Consultant Urologist & Clinical Senior Lecturer, Imperial College Healthcare NHS Trust
- Karen Wilkinson, Uro-Oncology CNS, University College London Hospitals NHS Trust
- Our Specialist Nurses
- Our volunteers.


